When diagnosed with coronary heart disease or discovering serious blockages in the coronary arteries, doctors often recommend Percutaneous Coronary Intervention (PCI) in the vernacular.
Upon hearing about the surgery, many patients may have questions: "Is the process complicated?", "Is the risk high?", and "Will the surgery ensure that there are no further issues in the future?" This article will comprehensively outline the entire process from pre-surgery examinations, surgical steps, inherent risks, to post-surgery recovery, helping you face the treatment with confidence.
"PCI" is a minimally invasive heart surgery that does not require opening the chest. During the procedure, doctors use catheter techniques to inflate a balloon and place a stent at the site of the narrowed artery, reopening vessels blocked by plaque (accumulation of fat and cholesterol) and restoring normal blood flow to the heart muscle. This technique is widely recognized in the international medical community as an important method to treat coronary heart disease.
Not all patients with arterial blockages require immediate surgery. Doctors assess patients' clinical conditions, imaging results, and overall risks to make a comprehensive evaluation. Generally, it can be divided into two categories:

To ensure the surgery is safe and to minimize complications, patients undergoing non-emergency PCI must undergo a rigorous assessment process:
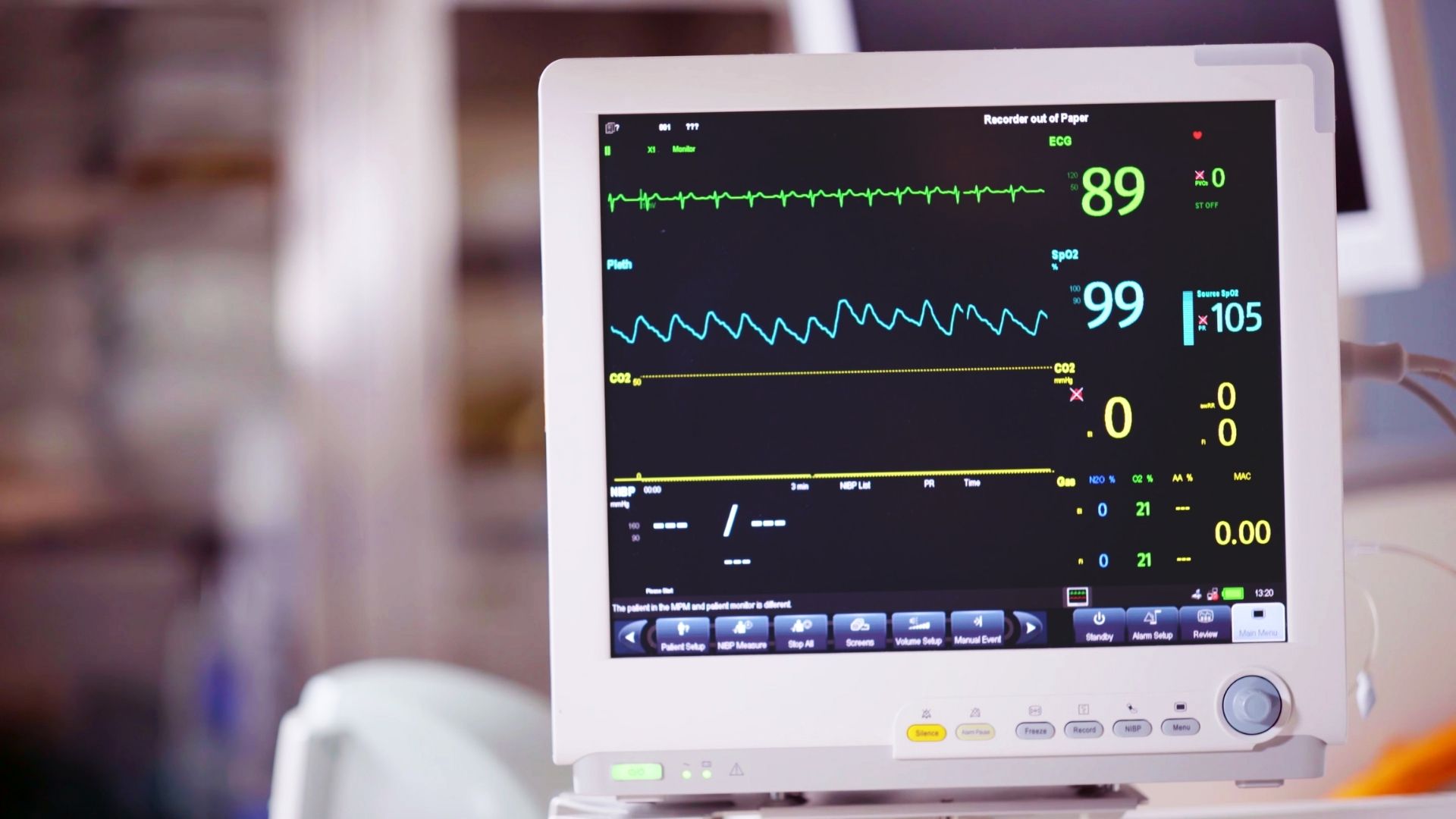
The surgery usually takes place under local anesthesia, with the patient fully conscious, lasting about 1 to 2 hours:
Not every patient requires the same approach; doctors will choose the most suitable treatment based on the vascular condition and clinical needs:

Although PCI is a highly safe minimally invasive procedure with an overall success rate of over 90%, there are still certain risks that need professional evaluation:
Successful surgery is just the first step; post-operative care is crucial to preventing a recurrence of cardiovascular issues:

A: This depends on the complexity of the vascular lesions. For patients with multiple vessel blockages, left main disease, or those with diabetes, surgical "bypass (CABG)" may offer better long-term patency. Doctors will discuss the most suitable option based on individual circumstances.
A: The surgery is performed under local anesthesia, so most of the time, there will only be a mild sensation. Some patients may feel temporary chest tightness or pressure when the balloon inflates, which typically subsides quickly.
A: Currently, most new generation drug-eluting stents are made of medical-grade stainless steel or alloys, and MRI examinations can generally be performed after implantation. However, you must present your stent implantation record card to radiology staff for verification before the exam.
Updated: 2025‑02
Disclaimer: The health information on this website has been reviewed by doctors from Chiron Medical Group. The above content is for general reference only and should not be regarded as medical advice. It is not a substitute for consultation with qualified healthcare professionals about your personal health condition.